Driving Sterilization Cost and Surgical Case Cycle Time Reduction
Background:
New payment initiatives such as Bundled Payments for Care Improvement (BPCI) as well as increased volumes in joint replacement surgeries are putting pressure on the need to reduce hospital costs for surgical procedures. Under the BPCI initiative, organizations enter into payment arrangements that include cost and performance accountability for episodes of care. In addition, OR on-time start and case cycle time are becoming critical in effectively managing the increase in surgical case volumes in Hospital ORs. Web-based coordination platforms that integrate with existing EMRs have shown promise in reducing OR sterilization costs and surgical case cycle time. By linking practices, hospitals and medical device vendors on a common platform, early collaboration on pre-operative surgical cases can help better meet BPCI goals while driving performance accountability through quality of care.
Objective:
The focus of the study was to measure the reduction in pre-operative planning time, instrument sterilization time & cost, and case cycle time across pre-op and post-op. The study provided the surgical practice team, hospital OR team and vendor with an integrated HIPAA compliant surgical case coordination platform to drive better planning of implant and instrumentation for upcoming surgeries. Cost and time reduction could help drive BPCI financial cost goal while maintaining and enhancing patient care.
Methods:
The study was done at Medical Center of Arlington in Arlington, Texas. The platform chosen for the trial was DocSpera, which allowed for surgical scheduling, pre-operative case planning and x-ray sharing with the OR team prior to surgery. For the study, Dr. Shane Seroyer, Medical Director and Orthopedic Surgeon focused on joint replacement – hip and knee replacement and revisions. He used DocSpera for pre-operative planning of all joint replacement surgeries. He worked with pre-operative nurse, physician assistant, material manager, sterilization manager and medical device representative on DocSpera’s platform to prepare upcoming surgical cases and drive advanced case visibility with the team. All members of his care team had access to DocSpera and were able to view all upcoming cases and templated x-rays to determine the type and size of implant required on average 3-4 weeks prior to surgery versus 5-7 days before.
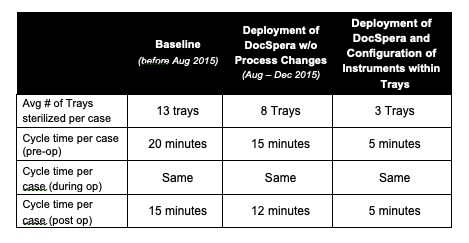
As part of the study, the team recorded the baseline of trays used per case and case cycle time across pre-op and post-op. For the first part of the study, conducted from August 2015 to May 2016, the team deployed DocSpera without any process changes. For second part of study, the team introduced instruments configuration based on upcoming case volumes and templated sizes visible in DocSpera to drive tray reduction.
Results:
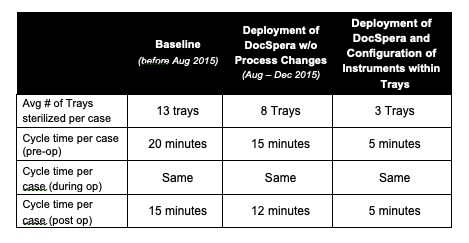
The advanced visibility and planning enabled by DocSpera, and subsequent configuration of instruments needed for specific cases, led to a reduction of trays brought to each surgical case from 13 down to 3 trays. By lowering the number of trays being used per case, the team was able to reduce the number of trays sterilized per case and decrease pre & post cycle time by 76% and 71%, respectively. The team was able to also reduce the amount of time it took to prepare instruments from the tray and assemble the instruments back in the tray for cleaning. This further led to a reduction in the average number of staff required to prepare and remove trays from 2 individuals down to 1.
In addition, fewer trays per case created significant space savings within the OR; the team reduced their use of tabletop space by 50% (from 6 cu ft. to 3 cu ft.), making it easier to operate in a smaller OR.
Conclusion:
DocSpera proved to be a major driver of efficiency during the study. From improved coordination between various surgical event providers, reduced administrative time required to book and reschedule cases, better visibility and communication regarding necessary surgical instruments, and time and space saved through the elimination of unnecessary materials, DocSpera delivered significant savings to the team over the course the study.
While efficiencies were pursued within the operating room suite, and many of them had to do with common objective projects, it was clear that utilizing DocSpera was one of the major drivers of efficiency.
Read More